Science on the Attack: The Hunt for a Coronavirus Vaccine (1)
/In my series of occasional posts showcasing science on the attack rather than under attack, this and the next blog post will review the current search for a vaccine against that unwelcome marauder, the coronavirus. This post examines vaccine approaches based on conventional, well-established techniques. The subsequent one will look at experimental technologies not yet approved for medical use.
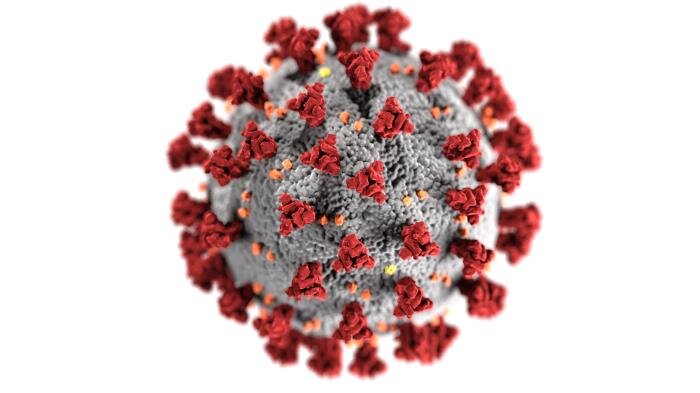
The coronavirus (SARS-CoV-2) is a very large, bristly molecule – with a genome twice as large as that of influenza – studded with spiky flower-like proteins as seen in red in the figure below. It tricks cells in the body into letting it in through a cellular door: a cup-like protein called an ACE2 receptor, which forms part of the nervous system and regulates bodily processes such as blood pressure and inflammation. Latching on to the receptor enables the virus to penetrate the host cell membrane and hijack the cell’s replication machinery, making copies of itself that then wreak havoc throughout the body.
The main function of the body’s immune system is to detect and annihilate invaders such as foreign bacteria and viruses like SARS-CoV-2. First, immune system scouts known as phagocytes – a type of white blood cell – recognize and digest intruder cells. The phagocyte surface then displays a flag or protein fragment of the bacteria or virus, called an antigen, that signals the foreigner’s identity. Other white blood cells called T cells identify the antigen, prompting the immune system arsenal to unleash one of two types of weapon against the assailant.
The two weapons are a different kind of T cell that homes in on infected cells and kills them, and yet another type of white blood cell called a B cell that produces disease fighting antibodies. Antibodies are specialized Y-shaped proteins with a search-and-destroy mission, either inactivating invasive cells directly or tagging them for elimination by phagocytes or other immune system killer cells. Coronavirus vaccines under development include both those that stimulate antibody production, and those that generate copious quantities of T cells.
Most of today’s vaccines utilize the virus itself. This can be in the form of a killed-virus vaccine, which is produced by growing live virus and then inactivating it chemically, or an attenuated live-virus vaccine, in which live virus is weakened below the level where it can normally cause disease. Both types of vaccine induce the immune system to churn out antibodies.
The measles-mumps-rubella (MMR) vaccine is an example of a weakened virus vaccine; most flu shots are the inactivated type. An inactivated coronavirus vaccine is now in Phase III efficacy testing by Chinese company Sinovac.
Attracting more attention for SARS-CoV-2 are so-called viral vector vaccines. As indicated in the next figure, these are vaccines in which a “guest” virus such as measles (left) or adenovirus (right), which causes upper respiratory infections and related illnesses, is genetically engineered with the gene for the coronavirus spike protein. Key genes in the guest virus are usually disabled so it can’t replicate, but the piggybacking coronavirus gene is unloaded inside the body’s cells, generating antibodies that combat the coronavirus invasion.
CREDIT: SPRINGER NATURE
The only vaccine currently approved for Ebola is a viral vector vaccine manufactured by Johnson & Johnson, who also have a coronavirus vaccine in the works. But the most advanced coronavirus effort is that of the University of Oxford together with AstraZeneca, who have Phase III trials of a viral vector vaccine well underway.
A third class of defense against the virus using established technologies is protein-based vaccines. Some protein-based vaccines contain fragments of the coronavirus spike protein, or of an important part of it known as the receptor binding domain. The fragments can’t cause disease because they’re not the actual virus, but the immune system is still able to recognize them as coronavirus proteins – triggering production of antibodies. Other protein-based vaccines contain a protein shell that mimics just the outer coat of the coronavirus, so again isn’t infectious but induces antibody production.
Current vaccines for shingles and human papillomavirus (HPV) are in this category. Several companies have Phase I or Phase II trials of a protein-based coronavirus vaccine in progress.
In the next post I’ll review experimental genetic vaccines for the coronavirus, which are based on antibodies, and newer candidates based on a strong T-cell response.
Next: Science on the Attack: The Hunt for a Coronavirus Vaccine (2)